Sid Stacey MHSc, Alex Drossos MD, Jennifer Brash MD
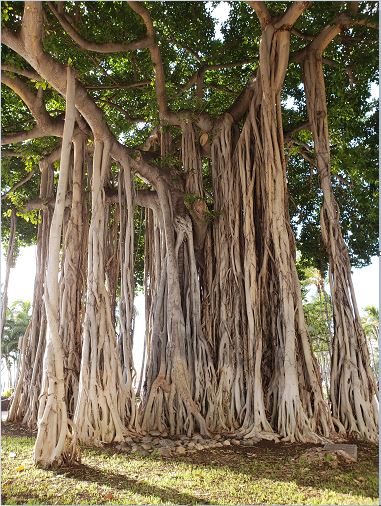
Image courtesy: Ana Hategan
Organizational culture, design, and leadership play a fundamental role in influencing sustainable medicine through promotion of wellness and resilience. The environment in which trainees learn and physicians provide clinical care is fundamentally influenced by leadership approaches to organizational design, culture, values, management style and approaches to multidisciplinary teams. These attributes shape the environment within which health professionals work and patient care is provided. Shanafelt et al (2017) identify several organizational strategies to promote engagement and reduce physician burnout, including:
Practicing resilience in the area of sustainable medicine requires organizations to promote a culture of engagement while at the same time minimize factors responsible for burnout. The Canadian Medical Association National Physician Health Survey found that physicians with five or fewer years in practice were more likely to experience burnout compared to all other physicians (CMA, 2018). Similarly, physicians who practiced in hospital settings had increased chances of experiencing lower social and psychological wellbeing. Concerning was the finding that burnout, depression, and lifetime suicidal ideation were higher among residents than practicing physicians and higher among women than men (CMA, 2018). In terms of help seeking, 81% of physicians surveyed reported that they were aware of physician health program services, but only 15% reported that they had accessed a physician health service program in the past five years (CMA, 2018). Healthcare organizations need to be proactive in designing physician health support programs and eliminating barriers to seeking help.
A growing number of healthcare organizations are focused on promoting the concept of resilience. The Institute of Healthcare Improvement has expanded the concept of Triple Aim, which includes enhancing the patient experience, population health management and cost efficient care to include the vital link among physician wellness, job satisfaction, and quality of care provided (Bodenheimer, 2014). Physician health promotion is informally known as “the fourth aim” which is oriented to improve the work life of clinicians and staff. Bodenheimer (2014) identifies that burnout is characterized by:
The concept of organizational resilience typically refers to the adaptive resources and ability of individuals to preserve a healthy relationship between individuals and their work in a changing environment (Rocha et al, 2015). Organizational resilience is an important concept that helps counter the reality that medicine often rewards excessive work. Multiple organizational pressures can generate workload imbalances for physicians and in more extreme cases can result in burnout. Early mentorship is essential to promote job satisfaction, team development, and meaning in work for both learners and staff physicians. Concomitantly, examining work and evaluating priorities are essential components of self-assessment, along with having early conversations about choosing your career path and ensuring professional and community supports are in place for optimal work-life balance.
Physician job satisfaction and wellbeing is a function of clearly defined roles, supportive organizational cultures, effective leadership and flexibility to ensure proper work-life balance is maintained. The Canterbury District Health Board, located in New Zealand/Aotearoa, introduced a comprehensive staff wellbeing program that included 26 wellbeing workshops and health and resilience sessions after the 2012 earthquake to ensure that physicians and staff had comprehensive supports to facilitate their adaptation and the provision of patient focused care (Manchester, 2015). This ultimately resulted in a resilience coordinator being appointed and a board governance committee to help support employee wellbeing and resilience and fostered organizational trust along with physician and employee commitment.
Job flexibility, leadership and growth opportunities, supportive administration and common vision are recognized as important factors that influence workload, job demands, and physician wellbeing (Getzin et al, 2016). Other personal factors such as supportive family and good work-life balance are foundational components of managing workload and job demands. Organizational leadership has an important responsibility to ensure that workload and job demands are reasonable and on-call schedules are realistic and achievable. Building staff resilience was a foundational strategy in the Canterbury District Health Board in New Zealand which helped generate an environment where the organization worked to achieve strong work-life balance for its physicians and hospital staff premised on the strategic understanding that staff wellbeing is a fundamental prerequisite to optimal patient-centred care (Manchester, 2015).
Learners identify early on the importance of protected academic time such as allocating half to a full day during the week for learning and academic development as important in balancing clinical responsibilities and educational requirements (Sharp & Burkart, 2017). Similarly, ensuring time has been allocated for self-care is often identified as an important work-life balance issue. Learners identify that supervisors who provide comprehensive support and supervision are an essential attribute of achieving work-life balance. Similarly, adherence to post call expectations where residents are relieved of clinical duties creates an environment in which call expectations are deemed more reasonable. Organizational and provincial policies or regulations such as parental leave contribute to healthy work environments.
Organizational leaders have a duty and responsibility to ensure that clinical teams are efficiently organized and have the resources necessary to provide optimal patient-centred care (Edrees et al, 2016). The growing gap between societal expectations and professional reality creates the climate in which 46% of physicians in the United States experience symptoms of burnout (Bodenheimer, 2014). Healthcare leaders have a critical role in ensuring that this gap is reduced and that healthcare resources are effectively aligned to support the provision of patient-centered care. Logistics and support issues are important as well. Residents who have hospital space allocated to them find it extremely beneficial to support their clinical and academic responsibilities (Sharp & Burkart, 2017). Other support policies such as residents doing electives out of town and not being required to “pay back” call expectations is an example of a policy to help generate healthy work-life balance.
Meaningful work is supported through core values such as health equity and social justice through medicine (Getzen et al, 2016). Organizational leaders have a critical role in influencing meaning in work for both practicing physicians and physicians in training. Resident choice in picking rotations and the ability to pursue unique interests have also been identified by residents as important factors in influencing their contribution (Sharp & Burkart, 2017). Learners need supervisors to engage with them about work and career trajectories and help draw out learner interest and clinical experiences. Peer and faculty mentorship is an essential contributor to work-life balance and meaning in work. The Institute for Health Care Improvement (Berwick, 2018) also encourages organizations to focus on developing strategies to foster joy in work. This requires spending time and effort in defining strategies that foster comprehensive staff wellbeing and engagement, which may include opportunities for leadership development. Engagement sessions with trainees that encourage resident physicians to identify activities that make work meaningful and those aspects of work that are not meaningful are helpful ways to focus attention on job satisfaction and work-life balance.
Healthy organizational culture is an essential responsibility of healthcare leaders. Culture comprises the values and basic assumptions and beliefs shared by individuals and groups and is expressed in the care and service provided by staff to patients (Rocha et al, 2016). Organizational leaders must provide opportunities for practicing physicians and physicians in training to reflect on culture and values. Typically, organizational values such as respect, equity, and diversity are defined by healthcare organizations and yet the strategies to promote these values may not be present. Organizations must ensure alignment of practices with their values and support practicing physicians and physicians in training to fully engage those values when practicing and participating in teams. Similarly, staff physicians or resident physicians that experience depression must be able to easily access confidential support and treatment. Resident physicians have identified that the PGY-2 year (the second year of post-graduate training) is an important year to reflect on values and often this is a period where the trainee can become more fatigued (Sharp et al, 2017). To help increase resilience and foster wellbeing, organizational practices that reinforce personal and professional values contribute to shaping a supportive culture.
Quality patient care and organizational performance are influenced by the amount of control and flexibility that staff, attending physicians, and resident physicians experience (Rosenstein, 2015). Residents who have control and flexibility ultimately report higher levels of satisfaction in training programs (Shanafelt et al, 2017). Assertiveness is also a concept that can be developed and taught combined along with tools to help generate healthy boundary management. Role clarity and role definition are essential elements in helping to effectively manage role expectations and interprofessional boundaries.
Organizational leaders must take a proactive role in fostering community at work and social support for staff, faculty members, and trainees. As previously mentioned, residents have identified that one of the most important factors in promoting trainee wellness is peer and faculty mentorship (Edrees et al, 2016). This includes fostering opportunities to connect with colleagues through retreats and welcome events and wellbeing workshops. Organizations need to ensure that physical design encourages connection spaces, lounges, and common areas where physicians and trainees can easily meet, fostering interdisciplinary collaboration and connection. Team meetings have the dual function of supporting clinical and organizational needs.
Work-life integration promotes balance amongst individual needs, work expectations, organizational factors, and cultural expectations (Shanafelt et al, 2017). Work-life integration is a concept that fosters optimal physician engagement and reduces the risk for burnout. Organizational factors that are key to work-life integration include policies that are supportive of staff such as reasonable workloads, supportive benefits, and wellness initiatives. Organizational leaders must ensure that staff and family wellbeing is embraced as a strategic organizational goal, backed up with a comprehensive staff wellbeing program including a focus on mental wellbeing and general resilience (Manchester, 2015). Similarly, empowering physicians to be able to shift work-life balance throughout their career creates healthy work-life integration throughout the career trajectory. Healthcare organizations need to recognize family achievement and collegiality just as much as they currently do teaching and research achievements. Healthy workplaces intentionally create opportunities for colleagues to connect on a social basis and promote physician engagement in clinical and academic activities. These strategies cumulatively create the culture and climate to balance personal and professional responsibilities and generate job satisfaction and joy in work.